Abstract
Background: Patients with sickle cell disease (SCD) are more likely to require surgical procedures, and to have post-operative complications compared to the general population. The TAPS trial demonstrated that pre-operative transfusion is associated with a 3.8-fold reduction in peri-operative complications in patients with SCD. Pre-operative exchange transfusion has not been shown to have benefit over simple top-up transfusion.
Patients with SCD may have baseline hemoglobin levels higher than the usual 60-80 g/L for a variety of reasons including; non-hemoglobin SS genotype SCD, co-inheritance of deletion(s) in alpha globin genes, hereditary persistence fetal hemoglobin, and hydroxyurea (HU) use. It is less clear whether patients with pre-operative hemoglobin levels > 90 g/L would also benefit from pre-operative transfusions. Previous studies of pre-operative transfusions in SCD have largely not captured these patients, in part due to low HU uptake at the time of the study and exclusion of non-hemoglobin SS SCD.
We conducted a retrospective cohort study to assess the role of pre-operative transfusion in patients with SCD and a high baseline hemoglobin.
Methods: 1304 patients seen at The Hospital for Sick Children, Toronto between 2007 and 2017 were assessed for eligibility. Patients were included if they: had a baseline hemoglobin ≥ 90 g/L, were 1-18 years of age at the time of surgery, had a diagnosis of hemoglobin SS, SC, Sβ+-thalassemia or Sβ0-thalassemia SCD subtypes, and had a low or medium risk elective surgery under a general anesthetic. Surgeries were classified according to the Co-operative Study of Sickle Cell Disease. Post-operative complications were defined as one or more of the following within 30 days of surgery: fever, vaso-occlusive crisis (VOC), infection, bleeding requiring transfusion, acute chest syndrome (ACS), stroke, intensive care admission (ICU), emergency room visit after discharge, readmission to hospital after discharge, or death. The incidence of postoperative complications for those with a baseline hemoglobin ≥90 g/L was compared between those who received a transfusion and those who did not. To estimate the adjusted effect of pre-operative transfusion on the risk of developing post-operative complications, a multi-variable logistic regression model was fitted using the change-in-estimate procedure, where variables with the strongest influence on the crude (unadjusted) estimate were included as model covariates (i.e. key confounders).
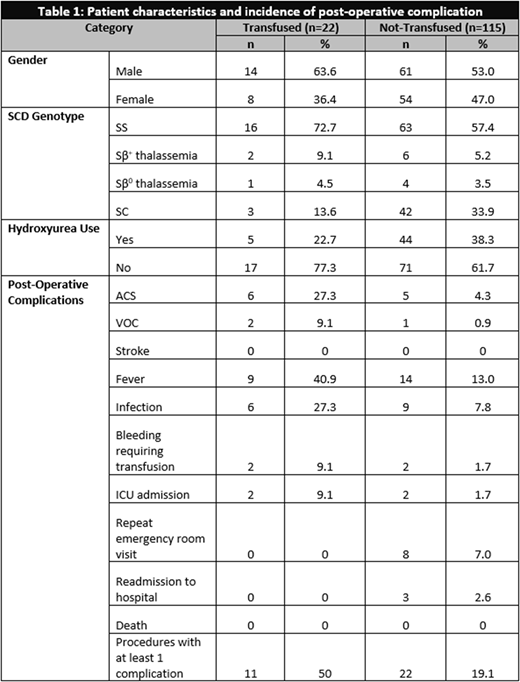
Results: 117 patients with a hemoglobin ≥90 g/L underwent a total of 137 procedures. The most frequent procedures included were: tonsillectomies/adenoidectomies (26), cholecystectomies (25), splenectomies (20), and umbilical hernia repairs (11).
There were 22 procedures (16%) where a pre-operative transfusion was administered. All patients received simple top-up transfusions. Of these, 11 (50%) encountered at least one post-operative complication. In contrast, 22/115 (19.1%) procedures without a pre-operative transfusion experienced a post-operative complication. There was an increased risk of post-operative complications in the group that was transfused (p=0.003, OR=4.2, 95% CI 1.6-11). Adjusting for two key confounders identified during the modeling process (splenectomy and prior ACS), pre-operative transfusion was again found to be associated with an increased risk of post-operative complications (p=0.017, OR=3.6, 95% CI 1.2-9.2). The characteristics of these patients and the incidence and distribution of post-operative complications are shown in Table 1.
Conclusion: Patients with SCD and a baseline hemoglobin ≥90 g/L who receive a pre-operative top-up transfusion have an increased risk of post-operative complications compared to those who are not transfused. In low and medium risk surgeries, a policy of withholding transfusions for such patients may be considered. Prospective studies validating these findings are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.